
“The UroLift clinical publication record is flawless. Every patient treated under a clinical protocol appears in at least one peer-reviewed publication. The outcomes from the numerous studies are consistent, demonstrating rapid relief within two weeks and sustained improvement in symptoms, quality of life and urinary flow.”
- Claus Roehrborn, MD
Urologist, USA
*Dr Roehrborn is a paid consultant of Neotract|Teleflex
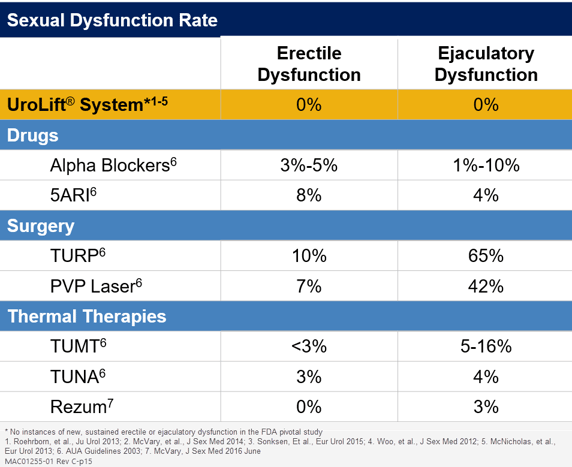
Clinical results from over 28 peer-reviewed publications demonstrate that treatment with the UroLift System offers rapid and significant improvements in symptoms, urinary flow and quality of life sustained through five years.1 Compared to medications, the UroLift System has demonstrated a more positive effect on quality of life for patients.1 The UroLift System treatment preserves sexual function and avoids complications typically associated with other BPH procedures.1,2,4,21*
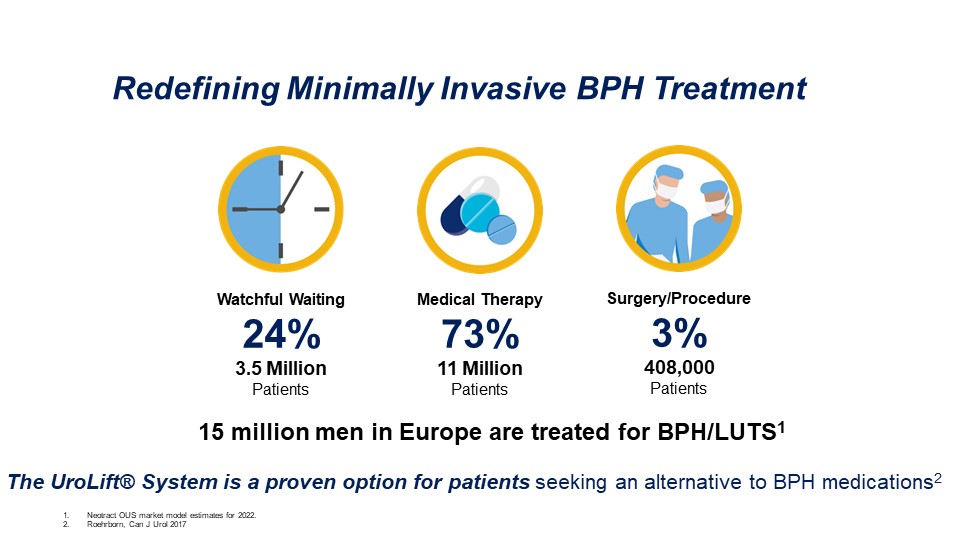
Most patients living with BPH take prescription medications, but these medications can become a lifelong burden. In a recent men’s health survey, two out of three patients reported frustration with their current BPH prescription.7 These patients have been unwilling to consider a surgical procedure due to the perceived risks and invasive nature of the standard options.
Now, urologists can offer men the UroLift System treatment—a BPH solution with a low risk profile to improve their patient’s quality of life.4
Patients on BPH Medications Are Not Satisfied
Surgery is a Big Step for Patients
Even Watchful Waiting Comes with Risks
In a global survey of 13,618 men age 40-80 across 29 countries, 23.8%-74.6% rated sex as being very to extremely important.18 Erectile dysfunction contributes to anxiety, depression, loss of self-esteem and diminished quality of life so preserving erectile function significantly impacts quality of life in BPH patients.19 In choosing a BPH treatment, it is important to consider the impact ejaculatory dysfunction and sexual function has on patient satisfaction.
*no new onset, sustained erectile or ejaculatory disfunction
Improvement in LUTS, as seen through average reduction in IPSS (International Prostate Symptom Score), has been consistent across the various studies, showing rapid relief within two weeks and sustained effect through five years.1 IPSS improvement at one year is better than seen with medications.2,4
Quality of life also improved significantly, with the IPSS QOL and BPH Impact Index maintaining 50% and 52% improvements, respectively at five years, p<0.0001.1
In addition to improving LUTS, the UroLift System treatment has demonstrated significant average improvement in peak urinary flow rate (Qmax) of 3.5 mL/sec (44%) that was sustained to five years, p<0.0001.1
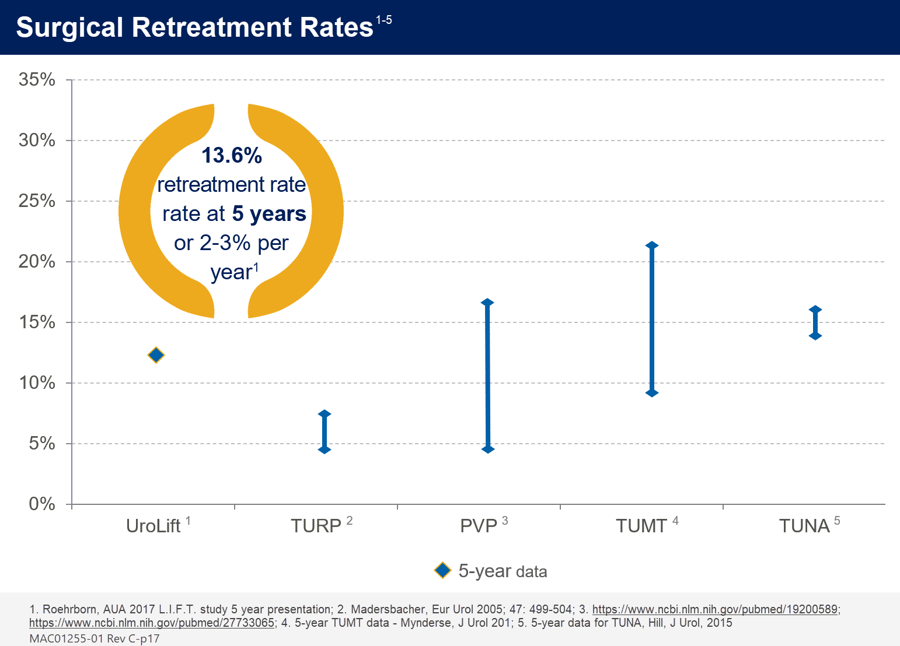
The rate of surgical intervention for failure to cure with the UroLift System remains low for a BPH procedure, with approximately 13.6% over five years or about 2-3% per year.1 Over the first postoperative year, no additional surgical intervention was required for bladder neck contracture, bleeding, or stress incontinence in the pivotal study on UroLift System.4

Publication
Roehrborn, et al.The Prostatic Urethral Lift for the Treatment of Lower Urinary Tract Symptoms Associated with Prostate Enlargement Due to Benign Prostatic Hyperplasia: The L.I.F.T. Study 2013.

Publication
Roehrborn, et al. Five year results of the prospective randomized controlled prostatic urethral L.I.F.T. study. Canadian Journal of Urology 2017.
Source Information
** Dr Roehrborn is a paid consultant of Neotract | Teleflex
*No instances of new, sustained erectile or ejaculatory dysfunction in the LIFT pivotal study
Grosvenor House, Horseshoe Crescent, Old Town, Beaconsfield, Bucks, HP9 1LJ
© 2024 Teleflex Inc. All rights reserved. | Terms of Use | Internet Privacy Policy | Patient Safety | Imprint | Compliance
MCI-2022-0108